Contents
The Seventh Report of the Joint National Committee on This work was supported entirely by the National Heart, Lung, and Blood Institute. The Executive Committee, writing teams, and reviewers served as volunteers without remuneration. 
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES National Institutes of Health National Heart, Lung, and Blood Institute National High Blood Pressure Education Program NIH Publication No. 03-5233 December 2003 Abstract The “Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure” provides a new guideline for hypertension prevention and management. The following are the report’s key messages:
introduction For more than three decades, the National Heart, Lung, and Blood Institute (NHLBI) has coordinated the National High Blood Pressure Education Program (NHBPEP), a coalition of 39 major professional, public, and voluntary organizations and seven Federal Agencies. One important function is to issue guidelines and advisories designed to increase awareness, prevention, treatment, and control of hypertension (high blood pressure (BP)). Since the publication of the “Sixth Report of the Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 6)” released in 1997,1 many large-scale clinical trials have been published. The decision to appoint a JNC 7 committee was based on four factors: (1) publication of many new hypertension observational studies and clinical trials; (2) need for a new, clear, and concise guideline that would be useful for clinicians; (3) need to simplify the classification of blood pressure; and (4) clear recognition that the JNC reports were not being used to their maximum benefit. This JNC report is presented in two separate publications: a current, succinct, practical guide and a more comprehensive report to be published separately, which will provide a broader discussion and justification for the current recommendations. In presenting these guidelines, the committee recognizes that the responsible physician’s judgment is paramount in managing patients. Methodology Since the publication of the JNC 6 report, the NHBPEP Coordinating Committee (CC), chaired by the director of the NHLBI, has regularly reviewed and discussed the hypertension clinical trials at its biannual meetings. In many instances, the principal investigator of the larger studies has presented the information directly to the CC. The committee’s presentations and reviews are summarized and posted on the NHLBI Web site.2 In agreeing to commission a new report, the Director requested that the CC members provide in writing a detailed rationale explaining the necessity to update the guidelines and to describe the critical issues and concepts to be considered for a new report. The JNC 7 chair was selected, plus a nine-member Executive Committee appointed entirely from the NHBPEP CC membership. The NHBPEP CC served as members of five writing teams, each of which was cochaired by two Executive Committee members. The concepts identified by the NHBPEP CC membership were used to develop the report outline. A timeline was developed to complete and publish the work in 5 months. Based on the identified critical issues and concepts, the Executive Committee identified relevant Medical Subject Headings (MeSH) terms and keywords to further review the scientific literature. These MeSH terms were used to generate MEDLINE searches that focused on English language peer-reviewed scientific literature from January 1997 through April 2003. Various systems of grading the evidence were considered, and the classification scheme used in the JNC 6 report and other NHBPEP clinical guidelines was selected3,4 which classifies studies in a process adapted from Last and Abramson.5 The Executive Committee met on six occasions, two of which included meetings with the entire NHBPEP CC. The writing teams also met by teleconference and used electronic communications to develop the report. Twenty-four drafts were created and reviewed in a reiterative fashion. At its meetings, the Executive Committee used a modified nominal group process to identify and resolve issues. The NHBPEP CC reviewed the penultimate draft and provided written comments to the Executive Committee. In addition, 33 national hypertension leaders reviewed and commented on the document. The NHBPEP CC approved the JNC 7 report. Classification of blood pressure Table 1 provides a classification of BP for adults ages 18 and older. The classification is based on the average of two or more properly measured, seated BP readings on each of two or more office visits. In contrast to the classification provided in the JNC 6 report, a new category designated prehypertension has been added, and stages 2 and 3 hypertension have been combined. Patients with prehypertension are at increased risk for progression to hypertension; those in the 130–139/80–89 mmHg BP range are at twice the risk to develop hypertension as those with lower values.6 Cardiovascular disease risk Hypertension affects approximately 50 million individuals in the United States and approximately 1 billion worldwide. As the population ages, the prevalence of hypertension will increase even further unless broad and effective preventive measures are implemented. Recent data from the Framingham Heart Study suggest that individuals who are normotensive at age 55 have a 90 percent lifetime risk for developing hypertension.7 The relationship between BP and risk of CVD events is continuous, consistent, and independent of other risk factors. The higher the BP, the greater is the chance of heart attack, heart failure, stroke, and kidney disease. For individu Table 1. Classification and management of blood pressure for adults*
DBP, diastolic blood pressure; SBP, systolic blood pressure. Drug abbreviations: ACEI, angiotensin converting enzyme inhibitor; ARB, angiotensin receptor blocker; BB, beta-blocker; CCB, calcium channel blocker. * Treatment determined by highest BP category. † Initial combined therapy should be used cautiously in those at risk for orthostatic hypotension. ‡ Treat patients with chronic kidney disease or diabetes to BP goal of <130/80 mmHg. als 40–70 years of age, each increment of 20 mmHg in systolic BP (SBP) or 10 mmHg in diastolic BP (DBP) doubles the risk of CVD across the entire BP range from 115/75 to 185/115 mmHg.8 The classification “prehypertension,” introduced in this report (table 1), recognizes this relationship and signals the need for increased education of health care professionals and the public to reduce BP levels and prevent the development of hypertension in the general population.9 Hypertension prevention strategies are available to achieve this goal. (See “Lifestyle Modifications” section.) benefits of lowering blood pressure In clinical trials, antihypertensive therapy has been associated with reductions in stroke incidence averaging 35–40 percent; myocardial infarction, 20–25 percent; and heart failure, more than 50 percent.10 It is estimated that in patients with stage 1 hypertension (SBP 140–159 mmHg and/or DBP 90–99 mmHg) and additional cardiovascular risk factors, achieving a sustained 12 mmHg reduction in SBP over 10 years will prevent 1 death for every 11 patients treated. In the presence of CVD or target organ damage, only 9 patients would require such BP reduction to prevent a death.11 Table 2. Trends in awareness, treatment, and control of high blood pressure in adults ages 18–74* 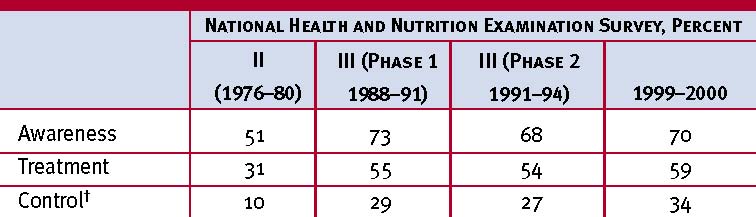 * High blood pressure is systolic blood pressure (SBP) ≥140 mmHg or diastolic blood pressure (DBP) ≥90 mmHg or taking antihypertensive medication. † SBP <140 mmHg and DBP <90 mmHg. Sources: Unpublished data for 1999–2000 computed by M. Wolz, National Heart, Lung, and Blood Institute; JNC 6.1 blood pressure control rates Hypertension is the most common primary diagnosis in America (35 million office visits as the primary diagnosis).12 Current control rates (SBP <140 mmHg and DBP <90 mmHg), though improved, are still far below the Healthy People 2010 goal of 50 percent; 30 percent are still unaware they have hypertension. (See table 2.) In the majority of patients, controlling systolic hypertension, which is a more important CVD risk factor than DBP except in patients younger than age 5013 and occurs much more commonly in older persons, has been considerably more difficult than controlling diastolic hypertension. Recent clinical trials have demonstrated that effective BP control can be achieved in most patients who are hypertensive, but the majority will require two or more antihypertensive drugs.14,15 When clinicians fail to prescribe lifestyle modifications, adequate antihypertensive drug doses, or appropriate drug combinations, inadequate BP control may result. accurate blood pressure measurement in the office The auscultatory method of BP measurement with a properly calibrated and validated instrument should be used.16 Persons should be seated quietly for at least 5 minutes in a chair (rather than on an exam table), with feet on the floor, and arm supported at heart level. Measurement of BP in the standing position is indicated periodically, especially in those at risk for postural hypotension. An appropriate-sized cuff (cuff bladder encircling at least 80 percent of the arm) should be used to ensure accuracy. At least two measurements should be made. SBP is the point at which the first of two or more sounds is heard (phase 1), and DBP is the point before the disappearance of sounds (phase 5). Clinicians should provide to patients, verbally and in writing, their specific BP numbers and BP goals. ambulatory blood pressure monitoring Ambulatory blood pressure monitoring (ABPM)17 provides information about BP during daily activities and sleep. ABPM is warranted for evaluation of “white-coat” hypertension in the absence of target organ injury. It is also helpful to assess patients with apparent drug resistance, hypotensive symptoms with antihypertensive medications, episodic hypertension, and autonomic dysfunction. The ambulatory BP values are usually lower than clinic readings. Awake, individuals with hypertension have an average BP of more than 135/85 mmHg and during sleep, more than 120/75 mmHg. The level of BP measurement by using ABPM correlates better than office measurements with target organ injury.18 ABPM also provides a measure of the percentage of BP readings that are elevated, the overall BP load, and the extent of BP reduction during sleep. In most individuals, BP decreases by 10 to 20 percent during the night; those in whom such reductions are not present are at increased risk for cardiovascular events. self-measurement of blood pressure BP self measurements may benefit patients by providing information on response to antihypertensive medication, improving patient adherence with therapy,19 and in evaluating white-coat hypertension. Persons with an average BP more than 135/85 mmHg measured at home are generally considered to be hypertensive. Home measurement devices should be checked regularly for accuracy. patient evaluation Evaluation of patients with documented hypertension has three objectives:
Table 3. Cardiovascular risk factors Table 4. Identifiable causes of hypertension Sleep apnea Hypertension* Cigarette smoking Obesity* (body mass index ≥30 kg/m2) Physical inactivity Dyslipidemia* Diabetes mellitus* Microalbuminuria or estimated GFR <60 mL/min Age (older than 55 for men, 65 for women) Family history of premature cardiovascular disease (men under age 55 or women under age 65) Heart
GFR, glomerular filtration rate. * Components of the metabolic syndrome. Drug-induced or related causes (see table 9) Chronic kidney disease Primary aldosteronism Renovascular disease Chronic steroid therapy and Cushing’s syndrome Pheochromocytoma Coarctation of the aorta Thyroid or parathyroid disease include an appropriate measurement of BP, with verification in the contralateral arm; examination of the optic fundi; calculation of body mass index (BMI) (measurement of waist circumference also may be useful); auscultation for carotid, abdominal, and femoral bruits; palpation of the thyroid gland; thorough examination of the heart and lungs; examination of the abdomen for enlarged kidneys, masses, and abnormal aortic pulsation; palpation of the lower extremities for edema and pulses; and neurological assessment. Laboratory Tests and Other Diagnostic ProceduresRoutine laboratory tests recommended before initiating therapy include an electrocardiogram; urinalysis; blood glucose and hematocrit; serum potassium, creatinine (or the corresponding estimated glomerular filtration rate [GFR]), and calcium;20 and a lipid profile, after 9- to 12-hour fast, that includes high-density lipoprotein cholesterol and low-density lipoprotein cholesterol, and triglycerides. Optional tests include measurement of urinary albumin excretion or albumin/creatinine ratio. More extensive testing for identifiable causes is not indicated generally unless BP control is not achieved. treatment Goals of TherapyThe ultimate public health goal of antihypertensive therapy is the reduction of cardiovascular and renal morbidity and mortality. Since most persons with hypertension, especially those age >50 years, will reach the DBP goal once SBP is at goal, the primary focus should be on achieving the SBP goal. Treating SBP and DBP to targets that are <140/90 mmHg is associated with a decrease in CVD complications. In patients with hypertension and diabetes or renal disease, the BP goal is <130/80 mmHg.21,22 Lifestyle ModificationsAdoption of healthy lifestyles by all persons is critical for the prevention of high BP and is an indispensable part of the management of those with hypertension. Major lifestyle modifications shown to lower BP include weight reduction in those individuals who are overweight or obese,23,24 adoption of the Dietary Approaches to Stop Hypertension (DASH) eating plan25 which is rich in potassium and calcium,26 dietary sodium reduction,25–27 physical activity,28,29 and moderation of alcohol consumption. (See table 5.)30 Lifestyle modifications reduce BP, enhance antihypertensive drug efficacy, and decrease cardiovascular risk. For example, a 1,600 mg sodium DASH eating plan has effects similar to single drug therapy.25 Combinations of two (or more) lifestyle modifications can achieve even better results. Pharmacologic TreatmentThere are excellent clinical outcome trial data proving that lowering BP with several classes of drugs, including angiotensin converting enzyme inhibitors (ACEIs), angiotensin receptor blockers (ARBs), beta-blockers (BBs), calcium channel blockers (CCBs), and thiazide-type diuretics, will all reduce the complications of hypertension.10,31–37 Tables 6 and 7 provide a list of commonly used antihypertensive agents. Thiazide-type diuretics have been the basis of antihypertensive therapy in most outcome trials.37 In these trials, including the recently published Antihypertensive and Lipid Lowering Treatment to Prevent Heart Attack Trial (ALLHAT),33 diuretics have been virtually unsurpassed in preventing the cardiovascular complications of hypertension. The exception is the Second Australian National Blood Pressure trial which reported slightly better outcomes in White men with a regimen that began with an ACEI compared to one starting with a diuretic.36 Diuretics enhance the antihypertensive efficacy Table 5. Lifestyle modifications to manage hypertension*†
DASH, Dietary Approaches to Stop Hypertension. * For overall cardiovascular risk reduction, stop smoking. † The effects of implementing these modifications are dose and time dependent, and could be greater for some individuals. of multidrug regimens, can be useful in achieving BP control, and are more affordable than other antihypertensive agents. Despite these findings, diuretics remain underutilized.39 Thiazide-type diuretics should be used as initial therapy for most patients with hypertension, either alone or in combination with one of the other classes (ACEIs, ARBs, BBs, CCBs) demonstrated to be beneficial in randomized controlled outcome trials. The list of compelling indications requiring the use of other antihypertensive drugs as initial therapy are listed in table 8. If a drug is not tolerated or is contraindicated, then one of the other classes proven to reduce cardiovascular events should be used instead. Table 6. Oral antihypertensive drugs* Table 6. Oral antihypertensive drugs* (continued) Table 6. Oral antihypertensive drugs*(continued)
* In some patients treated once daily, the antihypertensive effect may diminish toward the end of the dosing interval (trough effect). BP should be measured just prior to dosing to determine if satisfactory BP control is obtained. Accordingly, an increase in dosage or frequency may need to be considered. These dosages may vary from those listed in the “Physicians Desk Reference, 57th ed.” † Available now or soon to become available in generic preparations. Source: Physicians' Desk Reference. 57 ed. Montvale, NJ: Thomson PDR, 2003 Table 7. Combination drugs for hypertension
* Drug abbreviations: BB, beta-blocker; ACEI, angiotensin converting enzyme inhibitor; ARB, angiotensin receptor blocker; CCB, calcium channel blocker. † Some drug combinations are available in multiple fixed doses. Each drug dose is reported in milligrams. Achieving Blood Pressure Control in Individual PatientsMost patients who are hypertensive will require two or more antihypertensive medications to achieve their BP goals.14,15 Addition of a second drug from a different class should be initiated when use of a single drug in adequate doses fails to achieve the BP goal. When BP is more than 20/10 mmHg above goal, consideration should be given to initiating therapy with two drugs, either as separate prescriptions or in fixed-dose combinations. (See figure 1.) The initiation of drug therapy with more than one agent may increase the likelihood of achieving the BP goal in a more timely fashion, but particular caution is advised in those at risk for orthostatic hypotension, such as patients with diabetes, autonomic dysfunction, and some older persons. Use of generic drugs or combination drugs should be considered to reduce prescription costs. Figure 1. Algorithm for treatment of hypertension 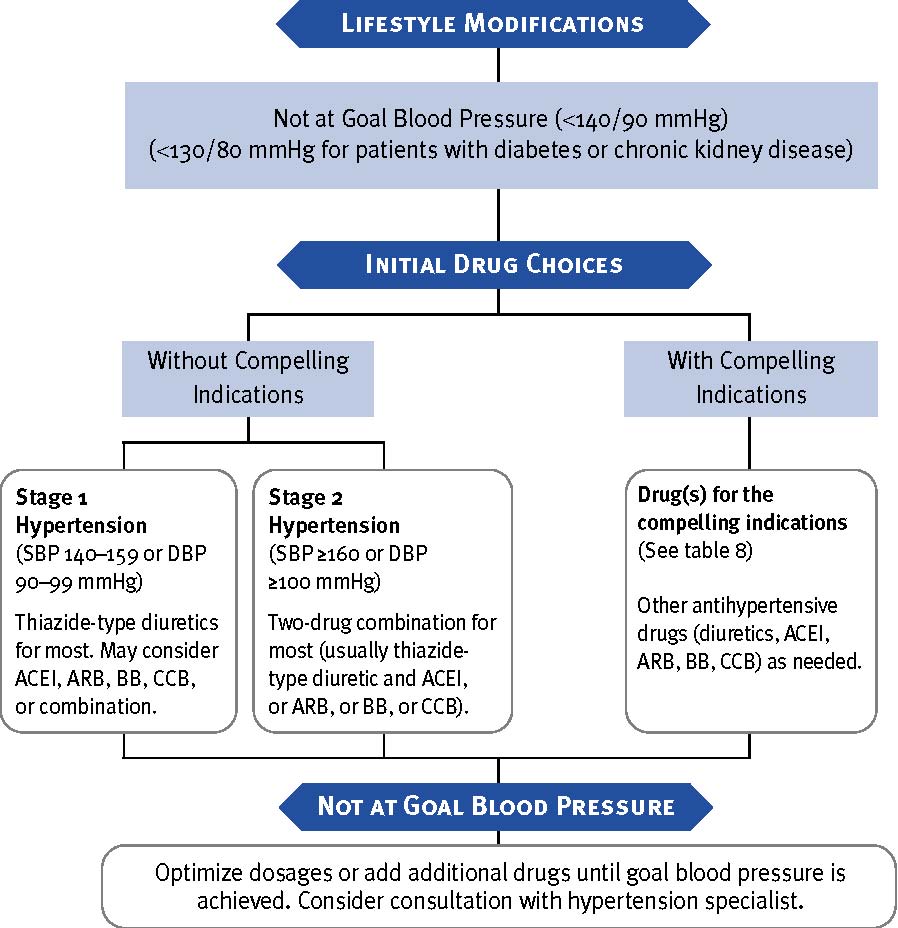 DBP, diastolic blood pressure; SBP, systolic blood pressure. Drug abbreviations: ACEI, angiotensin converting enzyme inhibitor; ARB, angiotensin receptor blocker; BB, beta-blocker; CCB, calcium channel blocker. Followup and MonitoringOnce antihypertensive drug therapy is initiated, most patients should return for followup and adjustment of medications at approximately monthly intervals until the BP goal is reached. More frequent visits will be necessary for patients with stage 2 hypertension or with complicating comorbid conditions. Serum potassium and creatinine should be monitored at least 1–2 times/year.60 After BP is at goal and stable, followup visits can usually be at 3- to 6-month intervals. Comorbidities, such as heart failure, associated diseases such as diabetes, and the need for laboratory tests influence the frequency of visits. Other cardiovascular risk factors should be treated to their respective goals, and tobacco avoidance should be promoted vigorously. Low-dose aspirin therapy should be considered only when BP is controlled, because the risk of hemorrhagic stroke is increased in patients with uncontrolled hypertension.61 special considerations The patient with hypertension and certain comorbidities requires special attention and followup by the clinician. Compelling IndicationsTable 8 describes compelling indications that require certain antihypertensive drug classes for high-risk conditions. The drug selections for these compelling indications are based on favorable outcome data from clinical trials. A combination of agents may be required. Other management considerations include medications already in use, tolerability, and desired BP targets. In many cases, specialist consultation may be indicated. Ischemic Heart DiseaseIschemic heart disease (IHD) is the most common form of target organ damage associated with hypertension. In patients with hypertension and stable angina pectoris, the first drug of choice is usually a BB; alternatively, long-acting CCBs can be used.1 In patients with acute coronary syndromes (unstable angina or myocardial infarction), hypertension should be treated initially with BBs and ACEIs,49 with addition of other drugs as needed for BP control. In patients with postmyocardial infarction, ACEIs, BBs, and aldosterone antagonists have proven to be most beneficial.50,52,53,62 Intensive lipid management and aspirin therapy are also indicated. Table 8. Clinical trial and guideline basis for compelling indications for individual drug classes
* Compelling indications for antihypertensive drugs are based on benefits from outcome studies or existing clinical guidelines; the compelling indication is managed in parallel with the BP. † Drug abbreviations: ACEI, angiotensin converting enzyme inhibitor; ARB, angiotensin receptor blocker; Aldo ANT, aldosterone antagonist; BB, beta-blocker; CCB, calcium channel blocker. ‡ Conditions for which clinical trials demonstrate benefit of specific classes of antihypertensive drugs. Heart FailureHeart failure (HF), in the form of systolic or diastolic ventricular dysfunction, results primarily from systolic hypertension and IHD. Fastidious BP and cholesterol control are the primary preventive measures for those at high risk for HF.40 In asymptomatic individuals with demonstrable ventricular dysfunction, ACEIs and BBs are recommended.52,62 For those with symptomatic ventricular dysfunction or end-stage heart disease, ACEIs, BBs, ARBs and aldosterone blockers are recommended along with loop diuretics.40–48 Diabetic HypertensionCombinations of two or more drugs are usually needed to achieve the target goal of <130/80 mmHg.21,22 Thiazide diuretics, BBs, ACEIs, ARBs, and CCBs are beneficial in reducing CVD and stroke incidence in patients with diabetes.33,54,63 ACEI- or ARB-based treatments favorably affect the progression of diabetic nephropathy and reduce albuminuria,55,56 and ARBs have been shown to reduce progression to macroalbuminuria.56,57 Chronic Kidney DiseaseIn people with chronic kidney disease (CKD), as defined by either (1) reduced excretory function with an estimated GFR below 60 ml/min per 1.73 m2 (corresponding approximately to a creatinine of >1.5 mg/dL in men or >1.3 mg/dL in women),20 or (2) the presence of albuminuria (>300 mg/day or 200 mg albumin/g creatinine), therapeutic goals are to slow deterioration of renal function and prevent CVD. Hypertension appears in the majority of these patients, and they should receive aggressive BP management, often with three or more drugs to reach target BP values of <130/80 mmHg.59,64 ACEIs and ARBs have demonstrated favorable effects on the progression of diabetic and nondiabetic renal disease.55–59,64 A limited rise in serum creatinine of as much as 35 percent above baseline with ACEIs or ARBs is acceptable and is not a reason to withhold treatment unless hyperkalemia develops.65 With advanced renal disease (estimated GFR <30 ml/min 1.73 m2, corresponding to a serum creatinine of 2.5–3 mg/dL), increasing doses of loop diuretics are usually needed in combination with other drug classes. Cerebrovascular DiseaseThe risks and benefits of acute lowering of BP during an acute stroke are still unclear; control of BP at intermediate levels (approximately 160/100 mmHg) is appropriate until the condition has stabilized or improved. Recurrent stroke rates are lowered by the combination of an ACEI and thiazide-type diuretic.35 Other Special Situations MinoritiesBP control rates vary in minority populations and are lowest in Mexican Americans and Native Americans.1 In general, the treatment of hypertension is similar for all demographic groups, but socioeconomic factors and lifestyle may be important barriers to BP control in some minority patients. The prevalence, severity, and impact of hypertension are increased in African Americans, who also demonstrate somewhat reduced BP responses to monotherapy with BBs, ACEIs, or ARBs compared to diuretics or CCBs. These differential responses are largely eliminated by drug combinations that include adequate doses of a diuretic. ACEI-induced angioedema occurs 2–4 times more frequently in African American patients with hypertension than in other groups.33 Obesity and the metabolic syndromeObesity (BMI >30 kg/m2) is an increasingly prevalent risk factor for the development of hypertension and CVD. The Adult Treatment Panel III guideline for cholesterol management defines the metabolic syndrome as the presence of three or more of the following conditions: abdominal obesity (waist circumference >40 inches in men or >35 inches in women), glucose intolerance (fasting glucose >110 mg/dL), BP >130/85 mmHg, high triglycerides (>150 mg/dL), or low HDL (<40 mg/dL in men or <50 mg/dL in women).66 Intensive lifestyle modification should be pursued in all individuals with the metabolic syndrome, and appropriate drug therapy should be instituted for each of its components as indicated. Left ventricular hypertrophyLeft ventricular hypertrophy (LVH) is an independent risk factor that increases the risk of subsequent CVD. Regression of LVH occurs with aggressive BP management, including weight loss, sodium restriction, and treatment with all classes of antihypertensive agents except the direct vasodilators hydralazine, and minoxidil.1,67 Peripheral arterial diseasePeripheral arterial disease (PAD) is equivalent in risk to IHD. Any class of antihypertensive drugs can be used in most PAD patients. Other risk factors should be managed aggressively, and aspirin should be used. Hypertension in older personsHypertension occurs in more than two-thirds of individuals after age 65.1 This is also the population with the lowest rates of BP control.68 Treatment recommendations for older people with hypertension, including those who have isolated systolic hypertension, should follow the same principles outlined for the general care of hypertension. In many individuals, lower initial drug doses may be indicated to avoid symptoms; however, standard doses and multiple drugs are needed in the majority of older people to reach appropriate BP targets. Postural hypotensionA decrease in standing SBP >10 mmHg, when associated with dizziness or fainting, is more frequent in older patients with systolic hypertension, diabetes, and those taking diuretics, venodilators (e.g., nitrates, alpha-blockers, and sildenafillike drugs), and some psychotropic drugs. BP in these individuals should also be monitored in the upright position. Caution should be used to avoid volume depletion and excessively rapid dose titration of antihypertensive drugs. DementiaDementia and cognitive impairment occur more commonly in people with hypertension. Reduced progression of cognitive impairment may occur with effective antihypertensive therapy.69,70 Hypertension in womenOral contraceptives may increase BP, and the risk of hypertension increases with duration of use. Women taking oral contraceptives should have their BP checked regularly. Development of hypertension is a reason to consider other forms of contraception. In contrast, menopausal hormone therapy does not raise BP.71 Women with hypertension who become pregnant should be followed carefully because of increased risks to mother and fetus. Methyldopa, BBs, and vasodilators are preferred medications for the safety of the fetus.72 ACEI and ARBs should not be used during pregnancy because of the potential for fetal defects and should be avoided in women who are likely to become pregnant. Preeclampsia, which occurs after the 20th week of pregnancy, is characterized by new-onset or worsening hypertension, albuminuria, and hyperuricemia, sometimes with coagulation abnormalities. In some patients, preeclampsia may develop into a hypertensive urgency or emergency and may require hospitalization, intensive monitoring, early fetal delivery, and parenteral antihypertensive and anticonvulsant therapy.72 Hypertension in children and adolescentsIn children and adolescents, hypertension is defined as BP that is, on repeated measurement, at the 95th percentile or greater adjusted for age, height, and gender.73 The fifth Korotkoff sound is used to define DBP. Clinicians should be alert to the possibility of identifiable causes of hypertension in younger children (i.e., kidney disease, coarctation of the aorta). Lifestyle interventions are strongly recommended, with pharmacologic therapy instituted for higher levels of BP or if there is insufficient response to lifestyle modifications.74 Choices of antihypertensive drugs are similar in children and adults, but effective doses for children are often smaller and should be adjusted carefully. ACEIs and ARBs should not be used in pregnant or sexually active girls. Uncomplicated hypertension should not be a reason to restrict children from participating in physical activities, particularly because long-term exercise may lower BP. Use of anabolic steroids should be strongly discouraged. Vigorous interventions also should be conducted for other existing modifiable risk factors (e.g., smoking). Hypertensive urgencies and emergenciesPatients with marked BP elevations and acute target-organ damage (e.g., encephalopathy, myocardial infarction, unstable angina, pulmonary edema, eclampsia, stroke, head trauma, life-threatening arterial bleeding, or aortic dissection) require hospitalization and parenteral drug therapy.1 Patients with markedly elevated BP but without acute target organ damage usually do not require hospitalization, but they should receive immediate combination oral antihypertensive therapy. They should be carefully evaluated and monitored for hypertension-induced heart and kidney damage and for identifiable causes of hypertension. (See table 4.) Additional Considerations in Antihypertensive Drug ChoicesAntihypertensive drugs can have favorable or unfavorable effects on other comorbidities. Potential favorable effectsThiazide-type diuretics are useful in slowing demineralization in osteoporosis. BBs can be useful in the treatment of atrial tachyarrhythmias/fibrillation, migraine, thyrotoxicosis (short term), essential tremor, or perioperative hypertension. CCBs may be useful in Raynaud’s syndrome and certain arrhythmias, and alpha-blockers may be useful in prostatism. Potential unfavorable effectsThiazide diuretics should be used cautiously in patients who have gout or who have a history of significant hyponatremia. BBs should generally be avoided in individuals who have asthma, reactive airways disease, or second or third degree heart block. ACEIs and ARBs should not be given to women likely to become pregnant and are contraindicated in those who are. ACEIs should not be used in individuals with a history of angioedema. Aldosterone antagonists and potassium-sparing diuretics can cause hyperkalemia and should generally be avoided in patients who have serum potassium values more than 5.0 mEq/L while not taking medications. improving hypertension control Adherence to RegimensBehavioral models suggest that the most effective therapy prescribed by the most careful clinician will control hypertension only if the patient is motivated to take the prescribed medication and to establish and maintain a health-promoting lifestyle. Motivation improves when patients have positive experiences with and trust in their clinicians. Empathy both builds trust and is a potent motivator.75 Patient attitudes are greatly influenced by cultural differences, beliefs, and previous experiences with the health care system.76 These attitudes must be understood if the clinician is to build trust and increase communication with patients and families. Failure to titrate or combine medications, despite knowing the patient is not at goal BP, represents clinical inertia and must be overcome.77 Decision support systems (i.e., electronic and paper), flow sheets, feedback reminders, and involvement of nurse clinicians and pharmacists can be helpful.78 The clinician and the patient must agree upon BP goals. A patient-centered strategy to achieve the goal and an estimation of the time needed to reach goal are important.79 When BP is above goal, alterations in the plan should be documented. BP self-monitoring can also be useful. Patients’ nonadherence to therapy is increased by misunderstanding of the condition or treatment, denial of illness because of lack of symptoms or perception of drugs as symbols of ill health, lack of patient involvement in the care plan, or unexpected adverse effects of medications. The patient should be made to feel comfortable in telling the clinician all concerns and fears of unexpected or disturbing drug reactions. The cost of medications and the complexity of care (i.e., transportation, patient difficulty with polypharmacy, difficulty in scheduling appointments, and life’s competing demands) are additional barriers that must be overcome to achieve goal BP. All members of the health care team (e.g., physicians, nurse case managers, and other nurses, physician assistants, pharmacists, dentists, registered dietitians, optometrists, and podiatrists) must work together to influence and reinforce instructions to improve patients’ lifestyles and BP control.80 Resistant HypertensionResistant hypertension is the failure to reach goal BP in patients who are adhering to full doses of an appropriate three-drug regimen that includes a diuretic. After excluding potential identifiable hypertension (see table 4), clinicians should carefully explore reasons why the patient is not at goal BP. (See table 9.) Particular attention should be paid to diuretic type and dose in relation to renal function. (See “Chronic Kidney Disease” section.) Consultation with a hypertension specialist should be considered if goal BP cannot be achieved. Table 9. Causes of resisitant hypertension Improper BP Measurement Volume Overload and Pseudotolerance
Drug-Induced or Other Causes
Associated Conditions
Identifiable Causes of Hypertension. (See table 4.) public health challenges and community programs Public health approaches, such as reducing calories, saturated fat, and salt in processed foods and increasing community/school opportunities for physical activity, can achieve a downward shift in the distribution of a population’s BP, thus potentially reducing morbidity, mortality, and the lifetime risk of an individual’s becoming hypertensive. This becomes especially critical as the increase in BMI of Americans has reached epidemic levels. Now, 122 million adults are overweight or obese, which contributes to the rise in BP and related conditions.81 The JNC 7 endorses the American Public Health Association resolution that the food manufacturers and restaurants reduce sodium in the food supply by 50 percent over the next decade. When public health intervention strategies address the diversity of racial, ethnic, cultural, linguistic, religious, and social factors in the delivery of their services, the likelihood of their acceptance by the community increases. These public health approaches can provide an attractive opportunity to interrupt and prevent the continuing costly cycle of managing hypertension and its complications. 
Evidence classification The studies that provided evidence supporting the recommendations of this report were classified and reviewed by the staff and the Executive Committee. The classification scheme is from the JNC 6 report.2 M Meta-analysis; use of statistical methods to combine the results from clinical trials RA Randomized controlled trials; also known as experimental studies RE Retrospective analyses; also known as case-control studies
 study abbreviations

Reference list
Discrimination Prohibited: Under provisions of applicable public laws enacted by Congress since 1964, no person in the United States shall, on the grounds of race, color, national origin, handicap, or age, be excluded from participation in, be denied the benefits of, or be subjected to discrimination under any program or activity (or, on the basis of sex, with respect to any education program or activity) receiving Federal financial assistance. In addition, Executive Order 11141 prohibits discrimination on the basis of age by contractors and subcontractors in the performance of Federal contracts, and Executive Order 11246 states that no federally funded contractor may discriminate against any employee or applicant for employment because of race, color, religion, sex, or national origin. Therefore, the National Heart, Lung, and Blood Institute must be operated in compliance with these laws and Executive Orders. Aram V. Chobanian, M.D. (Boston University Medical Center, Boston, MA) Executive Committee George L. Bakris, M.D. (Rush Presbyterian-St. Luke’s Medical Center, Chicago, IL); Henry R. Black, M.D. (Rush Presbyterian-St. Luke’s Medical Center, Chicago, IL); William C. Cushman, M.D. (Veterans Affairs Medical Center, Memphis, TN); Lee A. Green, M.D., M.P.H. (University of Michigan, Ann Arbor, MI); Joseph L. Izzo, Jr., M.D. (State University of New York at Buffalo School of Medicine, Buffalo, NY); Daniel W. Jones, M.D. (University of Mississippi Medical Center, Jackson, MS); Barry J. Materson, M.D., M.B.A. (University of Miami, Miami, FL); Suzanne Oparil, M.D. (University of Alabama at Birmingham, Birmingham, AL); Jackson T. Wright, Jr., M.D., Ph.D. (Case Western Reserve University, Cleveland, OH) Executive Secretary Edward J. Roccella, Ph.D., M.P.H. (National Heart, Lung, and Blood Institute, Bethesda, MD) National High Blood Pressure Education Program Coordinating Committee Participants Claude Lenfant, M.D., Chair (National Heart, Lung, and Blood Institute, Bethesda, MD); George L. Bakris, M.D. (Rush Presbyterian-St. Luke’s Medical Center, Chicago, IL); Henry R. Black, M.D. (Rush Presbyterian- St. Luke’s Medical Center, Chicago, IL); Vicki Burt, Sc.M., R.N. (National Center for Health Statistics, Hyattsville, MD); Barry L. Carter, Pharm.D. (University of Iowa, Iowa City, IA); Jerome D. Cohen, M.D. (Saint Louis University School of Medicine, St. Louis, MO); Pamela J. Colman, D.P.M. (American Podiatric Medical Association, Bethesda, MD); William C. Cushman, M.D. (Veterans Affairs Medical Center, Memphis, TN); Mark J. Cziraky, Pharm.D., F.A.H.A. (Health Core, Inc., Newark, DE); John J. Davis, P.A.-C. (American Academy of Physician Assistants, Memphis, TN); Keith Copelin Ferdinand, M.D., F.A.C.C. (Heartbeats Life Center, New Orleans, LA); Ray W. Gifford, Jr., M.D., M.S. (Cleveland Clinic Foundation, Fountain Hills, AZ); Michael Glick, D.M.D. (UMDNJ—New Jersey Dental School, Newark, NJ); Lee A. Green, M.D., M.P.H. (University of Michigan, Ann Arbor, MI); Stephen Havas, M.D., M.P.H., M.S. (University of Maryland School of Medicine, Baltimore, MD); Thomas H. Hostetter, M.D. (National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD); Joseph L. Izzo, Jr., M.D. (State University of New York at Buffalo School of Medicine, Buffalo, NY); Daniel W. Jones, M.D. (University of Mississippi Medical Center, Jackson, MS); Lynn Kirby, R.N., N.P., C.O.H.N.-S. (Sanofi- Synthelabo Research, Malvern, PA); Kathryn M. Kolasa, Ph.D., R.D., L.D.N. (Brody School of Medicine at East Carolina University, Greenville, NC); Stuart Linas, M.D. (University of Colorado Health Sciences Center, Denver, CO); William M. Manger, M.D., Ph.D. (New York University Medical Center, New York, NY); Edwin C. Marshall, O.D., M.S., M.P.H. (Indiana University School of Optometry, Bloomington, IN); Barry J. Materson, M.D., M.B.A. (University of Miami, Miami, FL); Jay Merchant, M.H.A. (Centers for Medicare & Medicaid Services, Washington, DC); Nancy Houston Miller, R.N., B.S.N. (Stanford University School of Medicine, Palo Alto, CA); Marvin Moser, M.D. (Yale University School of Medicine, Scarsdale, NY); William A. Nickey, D.O. (Philadelphia College of Osteopathic Medicine, Philadelphia, PA); Suzanne Oparil, M.D. (University of Alabama at Birmingham, Birmingham, AL); Otelio S. Randall, M.D., F.A.C.C. (Howard University Hospital, Washington, DC); James W. Reed, M.D., F.A.C.P., F.A.C.E. (Morehouse School of Medicine, Atlanta, GA); Edward J. Roccella, Ph.D., M.P.H. (National Heart, Lung, and Blood Institute, Bethesda, MD); Lee Shaughnessy (National Stroke Association, Englewood,CO); Sheldon G. Sheps, M.D. (Mayo Clinic, Rochester, MN); David B. Snyder, R.Ph., D.D.S. (Health Resources and Services Administration, Rockville, MD); James R. Sowers, M.D. (SUNY Health Science Center at Brooklyn, Brooklyn, NY); Leonard M. Steiner, M.S., O.D. (Eye Group, Oakhurst, NJ); Ronald Stout, M.D., M.P.H. (Procter and Gamble, Mason, OH); Rita D. Strickland, Ed.D., R.N. (New York Institute of Technology, Springfield Gardens, NY); Carlos Vallbona, M.D. (Baylor College of Medicine, Houston, TX); Howard S. Weiss, M.D., M.P.H. (Georgetown University Medical Center, Washington Hospital Center, Walter Reed Army Medical Center, Washington, DC); Jack P. Whisnant, M.D. (Mayo Clinic and Mayo Medical School, Rochester, MN); Laurie Willshire, M.P.H., R.N. (American Red Cross, Falls Church, VA); Gerald J. Wilson, M.A., M.B.A. (Citizens for Public Action on High Blood Pressure and Cholesterol, Inc., Potomac, MD); Mary Winston, Ed.D., R.D. (American Heart Association, Dallas, TX); Jackson T. Wright, Jr., M.D., Ph.D., F. A.C.P. (Case Western Reserve University, Cleveland, OH) Reviewers William B. Applegate, M.D., M.P.H. (Wake Forest University School of Medicine, Winston Salem, NC); Jan N. Basile, M.D., F.A.C.P. (Veterans Administration Hospital, Charleston, SC); Robert Carey, M.D., (University of Virginia Health System, Charlottesville, VA); Victor Dzau, M.D. (Brigham and Women’s Hospital, Boston, MA); Brent M. Egan, M.D. (Medical University of South Carolina, Charleston, SC); Bonita Falkner, M.D. (Jefferson Medical College, Philadelphia, PA); John M. Flack, M.D., M.P.H. (Wayne State University School of Medicine, Detroit, MI); Edward D. Frohlich, M.D. (Ochsner Clinic Foundation, New Orleans, LA); Haralambos Gavras, M.D. (Boston University School of Medicine, Boston, MA); Martin Grais, M.D. (Feinberg School of Medicine, Northwestern University, Chicago, IL); Willa A. Hsueh, M.D. (David Geffen School of Medicine, UCLA Department of Medicine, Los Angeles, CA); Kenneth A. Jamerson, M.D. (University of Michigan Medical Center, Ann Arbor, MI); Norman M. Kaplan, M.D. (University of Texas Southwestern Medical Center, Dallas, TX); Theodore A. Kotchen, M.D. (Medical College of Wisconsin, Milwaukee, WI); Daniel Levy, M.D. (National Heart, Lung, and Blood Institute, Framingham, MA); Michael A. Moore, M.D. (Dan River Region Cardiovascular Health Initiative Program, Danville, VA); Thomas J. Moore, M.D. (Boston University Medical Center, Boston, MA); Vasilios Papademetriou, M.D., F.A.C.P., F.A.C.C. (Veterans Affairs Medical Center, Washington, DC); Carl J. Pepine, M.D. (University of Florida, College of Medicine, Gainesville, FL); Robert A. Phillips, M.D., Ph.D. (New York University, Lenox Hill Hospital, New York, NY); Thomas G. Pickering, M.D., D.Phil. (Mount Sinai Medical Center, New York, NY); L. Michael Prisant, M.D., F.A.C.C., F.A.C.P. (Medical College of Georgia, Augusta, GA); C. Venkata S. Ram, M.D. (University of Texas Southwestern Medical Center and Texas Blood Pressure Institute, Dallas, TX); Elijah Saunders, M.D., F.A.C.C., F.A.C.P. (University of Maryland School of Medicine, Baltimore, MD); Stephen C. Textor, M.D. (Mayo Clinic, Rochester, MN); Donald G. Vidt, M.D. (Cleveland Clinic Foundation, Cleveland, OH); Myron H. Weinberger, M.D. (Indiana University School of Medicine, Indianapolis, IN); Paul K. Whelton, M.D., M.Sc. (Tulane University Health Sciences Center, New Orleans, LA) Staff Joanne Karimbakas, M.S., R.D. (Prospect Associates, Ltd., now part of American Institutes for Research Health Program, Silver Spring, MD) We appreciate the assistance of Carol Creech, M.I.L.S. and Gabrielle Gessner (Prospect Associates, Ltd., now part of American Institutes for Research Health Program, Silver Spring, MD). The National High Blood Pressure Education Program (NHBPEP) Coordinating Committee Member Organizations American Academy of Family Physicians American Academy of Neurology American Academy of Ophthalmology American Academy of Physician Assistants American Association of Occupational Health Nurses American College of Cardiology American College of Chest Physicians American College of Occupational and Environmental Medicine American College of Physicians-American Society of Internal Medicine American College of Preventive Medicine American Dental Association American Diabetes Association American Dietetic Association American Heart Association American Hospital Association American Medical Association American Nurses Association American Optometric Association American Osteopathic Association American Pharmaceutical Association American Podiatric Medical Association American Public Health Association American Red Cross American Society of Health-System Pharmacists American Society of Hypertension American Society of Nephrology Association of Black Cardiologists Citizens for Public Action on High Blood Pressure and Cholesterol, Inc. Hypertension Education Foundation, Inc. International Society on Hypertension in Blacks National Black Nurses Association, Inc. National Hypertension Association, Inc. National Kidney Foundation, Inc. National Medical Association National Optometric Association National Stroke Association NHLBI Ad Hoc Committee on Minority Populations Society for Nutrition Education The Society of Geriatric Cardiology Federal Agencies:Agency for Healthcare Research and Quality Centers for Medicare & Medicaid Services Department of Veterans Affairs Health Resources and Services Administration National Center for Health Statistics National Heart, Lung, and Blood Institute National Institute of Diabetes and Digestive and Kidney Diseases NIH Publication No. 03-5233 December 2003 Click on links for the procedures for specific instructions on initial reporting, medication discussion and followup procedures: List of Medical Problems |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Exam Info | Online Scheduling Info | Find AME | Pilot FAQs | Sport Pilots | Part 67 Medical Standards | Blood Pressure | Part 61 Flight Certification |DUI | Waivers
How Site Works | Online Scheduling | Update my Page | Links | Prices | Email | Pay Bill | AME FAQs | Trade Equipment | AME Guide
Pilot FAQs | AME FAQs | FAQ's By Medical Problem | Sport Pilot | Blood Pressure | Scheduling | Contact Us
Exam Info | Synopsis of Standards |CFR Part 67 | Exam Classes | Class 1 Requirements | Class 2 | Class 3 | Problem List | Waivers | Blood Pressure
subglobal6 link | subglobal6 link | subglobal6 link | subglobal6 link | subglobal6 link | subglobal6 link | subglobal6 link


